Table of Contents
Introduction
Suddenly losing someone to epilepsy is heartbreaking, especially when it happens without warning. This kind of tragedy is called sudep, which stands for Sudden Unexpected Death in Epilepsy. Many people with epilepsy and their families have never heard of sudep until it’s too late. That’s why this topic needs more attention. Sudep happens when a person with epilepsy dies suddenly, often during sleep or right after a seizure, and no other cause of death is found. It’s rare, but it’s real. Talking about sudep doesn’t mean living in fear. It means being informed and prepared. When people with epilepsy know the risk, they can take steps to stay safer. In this guide, we’ll explain what sudep is, why it happens, who is at risk, and what can be done to lower those risks. We’ll also answer common questions and share practical ways to help. Knowledge about sudep can save lives, and that’s the reason this information matters so much.
What Does Sudep Mean
Sudep stands for Sudden Unexpected Death in Epilepsy. It’s a medical term used when a person with epilepsy dies suddenly without any clear cause, such as injury, drowning, or heart failure. The person usually has a seizure shortly before the death, but not always. Most cases of sudep happen during sleep and are only discovered when the person doesn’t wake up. Doctors often don’t find any damage or exact reason why it happened. That’s what makes sudep so hard to understand and so painful for families. Even though it’s rare, sudep is the leading cause of death in people with uncontrolled epilepsy. Knowing what sudep means can help you ask better questions and make smart choices for better seizure management and safety.
Who Is at Risk of Sudep
Sudep can happen to anyone with epilepsy, but some people have a higher risk. People who have frequent seizures, especially generalized tonic-clonic seizures, are more likely to experience sudep. These types of seizures involve full body convulsions and loss of consciousness. People who have seizures at night or live alone may also face higher risks. Here are risk factors connected to a higher chance of sudep: having uncontrolled epilepsy, not taking seizure medicine as prescribed, missing doctor visits, drinking alcohol or using drugs, not getting enough sleep, and having long-lasting or back-to-back seizures. If you or someone you know has epilepsy, talk to a doctor about these risks. Preventing sudden death often starts by improving seizure control and knowing your specific triggers and health history.
How Often Does Sudep Happen
Every year, about 1 in every 1,000 people with epilepsy will die from sudep. That number increases to 1 in 150 for people with difficult-to-control epilepsy or those with frequent seizures. Even though it’s rare, it’s still the number one epilepsy-related cause of death. One reason sudep deaths are underreported is because many doctors and hospitals don’t always recognize it or mention it in reports. Often, the only way to know if a death was caused by sudep is through a full autopsy, which isn’t always done. That means the actual number of sudep cases might be higher than we think. Sharing this information helps more people realize that while seizure control is essential, preventing sudep is just as important.
What Causes Sudep According to Experts
Researchers are still working to fully understand sudep, but several causes are possible. Most experts think sudep happens when a seizure affects the way the brain controls breathing or heart function. During or just after a seizure, the person may stop breathing, the heart may beat irregularly, or the brain may fail to wake the body up. One common theory is that seizures during sleep may cause a person to be facedown, making it hard to breathe. The airway can become blocked if no one is nearby to help. Some people think sudden heart rhythm changes might be responsible. Changes in oxygen, brain activity, or nerve functions could also play a role. Each person is different, and sudep likely involves more than one cause. This is why it’s important to stay informed and report all seizure activity to your health care provider.
How to Lower the Risk of Sudep
The first and best way to reduce the risk of sudep is to control seizures as much as possible. Take all seizure medications just as your doctor prescribes. Don’t skip doses. Go to your checkups, track your seizures, and tell your doctor right away if your seizures worsen or change. Making small changes can help a lot. Avoid your triggers, like lack of sleep or stress. Stay active and healthy through proper sleep, hydration, and nutrition. If your seizures happen mostly at night, don’t sleep alone. Use a seizure alert device or smart monitor that can wake someone if a seizure happens. Educate your family or roommates about seizure first aid. They can help you roll onto your side or call for help. These steps might sound small, but they can make a big difference in avoiding sudep and staying safer during seizures.
Why Sudep Is Often Overlooked
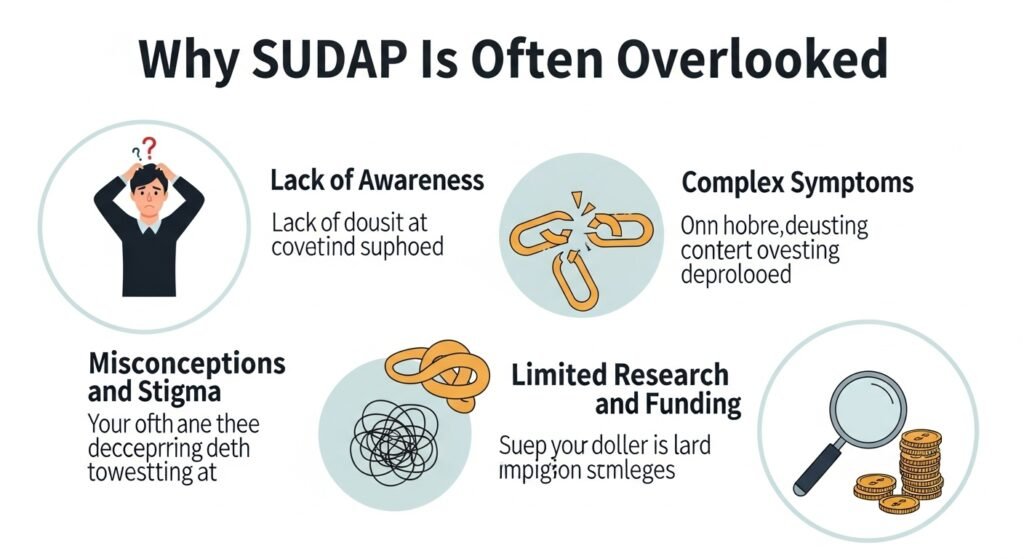
Many doctors and care teams don’t bring up sudep, even for patients who are at higher risk. This is partly because it’s rare, and no one wants to scare patients or families. Sometimes, medical professionals also feel uncomfortable talking about death, especially when there’s no guaranteed way to prevent it. But the truth is, learning about sudep helps people take practical steps to stay safer. People with epilepsy have the right to know all the facts. Families often say they wish they had been told about sudep earlier so they could watch for patterns, prepare for seizures at night, or take seizure medicine more seriously. Educating patients about sudep in a calm, honest way gives them power—not fear. The more we talk about it, the easier it becomes to prevent it and give others the chance to live long, healthy lives.
Sudep in Children and Young Adults
Sudep doesn’t just happen to adults—it can affect children and young people too. Although it’s not as common in kids, families should still be aware of it. Children with uncontrolled seizures, especially tonic-clonic ones, may have a higher risk. For teens and young adults, the risk becomes greater if they start skipping medications or stop going to regular doctor visits. It’s also common for young people to start living on their own, increasing the chance that seizures will go unnoticed. Parents and caregivers can help by keeping medication schedules consistent, using seizure tracking apps, and paying extra attention to nighttime safety. Wearing devices that detect movement during sleep is another good idea. By starting seizure education early in life, children with epilepsy can grow up more aware and independent, while still protected from the risk of sudep.
Technologies That Help Prevent Sudep
New technology is making it easier to monitor seizures and possibly lower the risk of sudep. Items like smartwatches, seizure-detection sensors, and sleep monitors can alert others when a seizure starts. Some wristbands check for motion, heart rate, or breathing changes. Bed alarms can detect when someone is shaking or moving too much in their sleep. There are even camera systems that watch for odd sleep patterns and send alerts. While these devices can’t stop a seizure or cure epilepsy, they can give you more time to respond—and response time means everything after a seizure. Talking to your doctor about these devices could be an important step if you’re concerned about nighttime seizures and the possibility of sudep.
The Role of Family and Caregivers in Sudep Prevention
Family and caregivers play a huge role in reducing the risks of sudep. They’re often the ones who notice seizure triggers, catch missing medications, and respond in emergencies. They can learn how to help during and after a seizure by taking a short seizure first aid course. Caregivers can also check if a person with epilepsy needs a seizure monitor for nighttime safety. Keeping contact with the person, especially if they live alone, is another way to increase safety. Sudep doesn’t happen often, but support from loved ones does lower the risk. The more involved and informed they are, the better chances a person with epilepsy has to stay safe every day.
Sudep Awareness in the Medical Community
The topic of sudep is gaining more attention in the medical world, but there’s still progress to be made. More epilepsy clinics are adding sudep to their patient education materials. Some hospitals are using posters and handouts to start open conversations. The goal is to make sudep a normal part of epilepsy talk—just like talking about medication or diet. Doctors are encouraged to introduce it during care planning, especially for people with frequent or uncontrolled seizures. Patients are encouraged to ask questions and take an active role in their care. When everyone from the medical team to the patient knows what sudep is, safer choices can follow. More research, better tools, and honest conversations will bring us closer to the day when sudep is no longer a leading cause of epilepsy deaths.
FAQs
1. What is sudep in simple words Sudep is a sudden, unexpected death in someone with epilepsy, usually after a seizure, with no other cause found.
2. Is sudep common Sudep is rare, but it’s the main cause of epilepsy-related death. The risk is higher in people with frequent or nighttime seizures.
3. Can sudep happen without a seizure Most sudep cases follow a seizure, especially tonic-clonic ones, but some may happen without warning.
4. Can children have sudep Yes, sudep can happen in children, especially those with uncontrolled seizures. It’s less common but still possible.
5. How can I prevent sudep You can lower your risk by taking medication, avoiding seizure triggers, using monitors, and not sleeping alone if you have severe seizures.
6. Should I be scared of sudep Being informed is better than being scared. Sudep is rare and understanding it helps you take steps to stay safe.
Conclusion
Learning about sudep might feel scary, but staying silent is far worse. Knowing this silent risk means we can do something about it. If you or someone you love has epilepsy, learning about sudep gives you the tools to lower risk, track seizures, and plan for safety. Even though we can’t prevent every sudden loss, we can change how we respond. Simple things like medicine reminders, avoiding sleep alone, and using seizure monitors can change everything. Families, doctors, and caregivers all play a part in reducing sudep risk. The more we talk about it, the more lives we can protect. Share this knowledge. Ask the hard questions. Keep learning. Because talking about sudep doesn’t take hope away—it gives it back. And for someone living with epilepsy, that hope could be life-saving.